The U.S. health innovation ecosystem stands as a global beacon, driving cutting-edge advancements in medicine and technology. Born from the urgent needs of World War II, this ecosystem has evolved into a robust public-private research partnership that leverages significant federal funding, particularly from agencies like the NIH. Yet, recent discussions around NIH funding cuts underscore the precarious nature of this financial support, which fuels biomedical innovation and drives new discoveries. Understanding the historical context of U.S. health innovations reveals the profound impact of wartime breakthroughs, including the mass production of penicillin, which reshaped medical science. Today, as technology in warfare continues to advance, the synergy between federal investment and private sector ingenuity remains critical to sustaining this pioneering spirit in healthcare.
The health innovation landscape in the United States is marked by dynamic collaborations between government entities and the private sector, often referred to as a public-private research collaboration. This collaborative framework has its roots in historical exigencies, notably during World War II, when rapid advancements were needed to address critical health challenges facing the military. The momentum created during this era birthed a thriving biomedical innovation system that remains influential today. As discussions around federal funding for research intensify, particularly in light of potential NIH budget reductions, it is essential to recognize the ongoing importance of sustained investment in health innovations. This cooperative model has not only enhanced the capabilities of the health sector but has also significantly advanced national defense and public health outcomes.
The Evolution of the U.S. Health Innovation Ecosystem
The U.S. health innovation ecosystem has undergone a remarkable transformation since its inception during the early 20th century, particularly amid the exigencies of World War II. Initially, this ecosystem was rudimentary, relying heavily on trial and error due to limited scientific understanding and funding. However, the stakes of the war prompted a structured collaboration between the government and academic institutions, leading to significant advancements in biomedical research and development. This public-private partnership laid the groundwork for the sophisticated innovation landscape we observe today. Through initiatives like the Office of Scientific Research and Development (OSRD), resources were pooled to mobilize scientists for urgent military needs, which inadvertently spurred civilian health breakthroughs that continue to shape contemporary medicine.
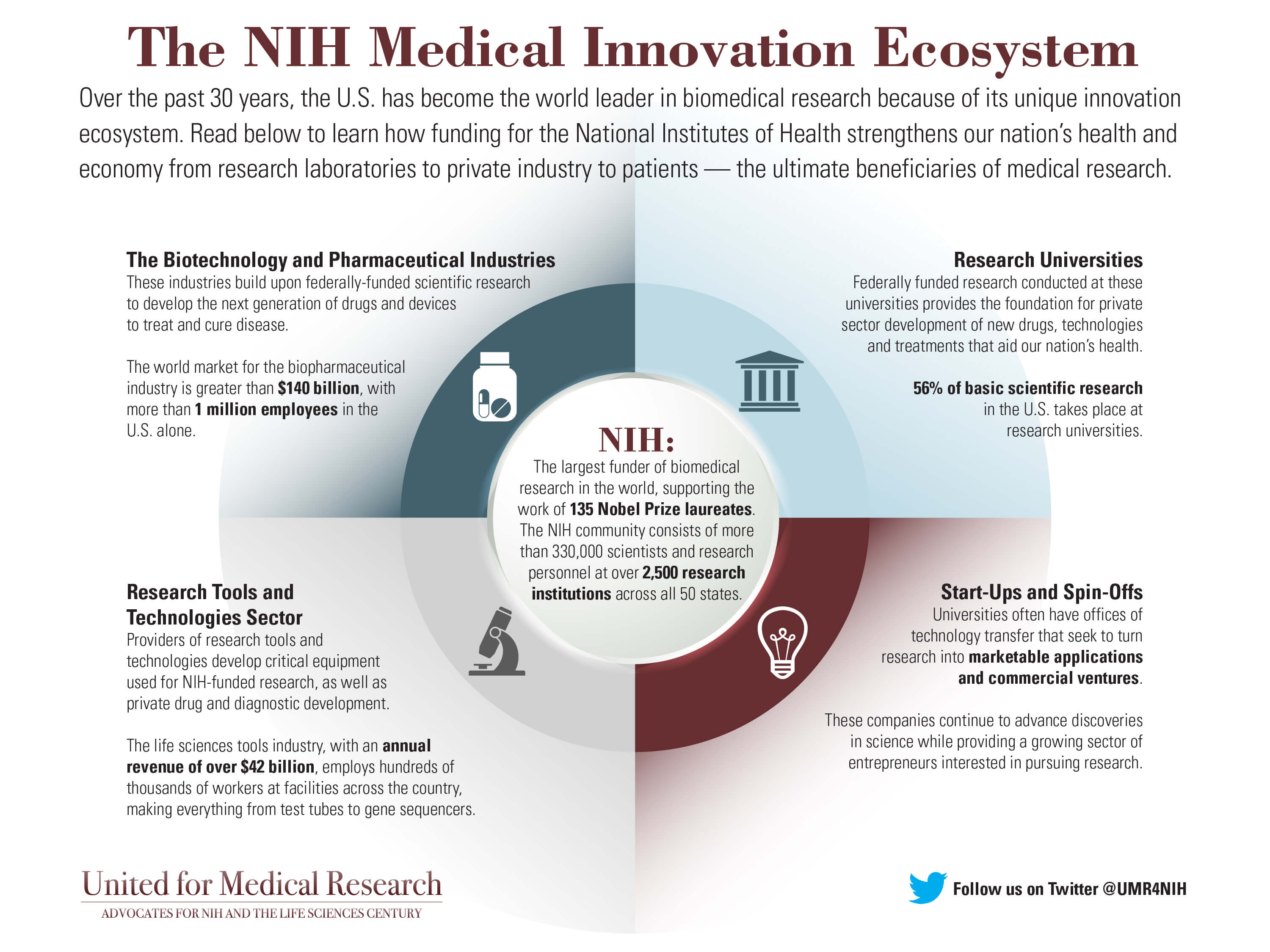
Today, the U.S. health innovation ecosystem stands as a global benchmark, underpinned by substantial investments in research from entities like the National Institutes of Health (NIH). This flourishing environment fosters advancements in areas such as biotechnology, pharmaceuticals, and medical devices, driving improvements in public health outcomes. The confluence of federal support, academic rigor, and entrepreneurial spirit has facilitated a vibrant landscape where scientific and technological innovation thrives. Consequently, the U.S. remains at the forefront of biomedical innovation, addressing ongoing and emergent health challenges with an adaptive and resilient research infrastructure.
Public-Private Research Partnerships in Health Innovation
Public-private research partnerships have been pivotal in shaping the trajectory of health innovation in the United States. These collaborations have enabled the pooling of expertise, resources, and funding, allowing for a more comprehensive approach to solving complex medical issues. The Foundation model involves not only federal entities like the NIH but also private-sector pharmaceutical companies, academic institutions, and nonprofit organizations aligning their objectives around common health challenges. By fostering an environment conducive to mutual benefit, these partnerships have historically driven breakthroughs in drug development, technology transfer, and clinical research, bolstering the effectiveness of the biomedical innovation system.
The urgency of health crises, reminiscent of the World War II era, has often catalyzed the formation of these partnerships. For instance, recent global health emergencies have necessitated swift collaborative efforts among academic researchers and private firms to accelerate vaccine development and deployment. The synergies created through such collaborations also facilitate access to cutting-edge technology, streamline regulatory processes, and improve the translation of scientific discoveries into viable treatments. As the landscape evolves, enhancing these partnerships is essential for sustaining the momentum of innovation within the health sector.
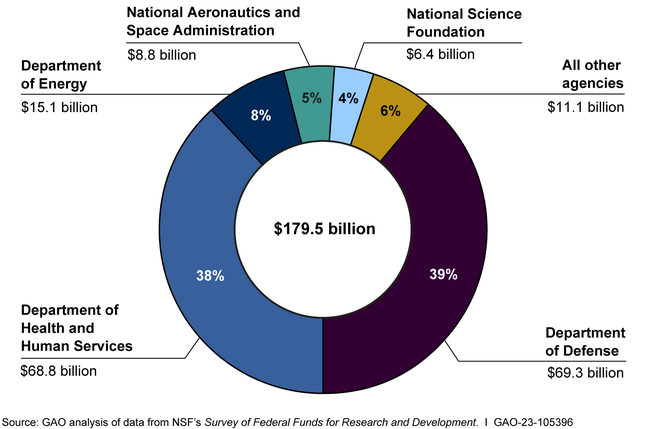
The Impact of NIH Funding on Biomedical Innovation
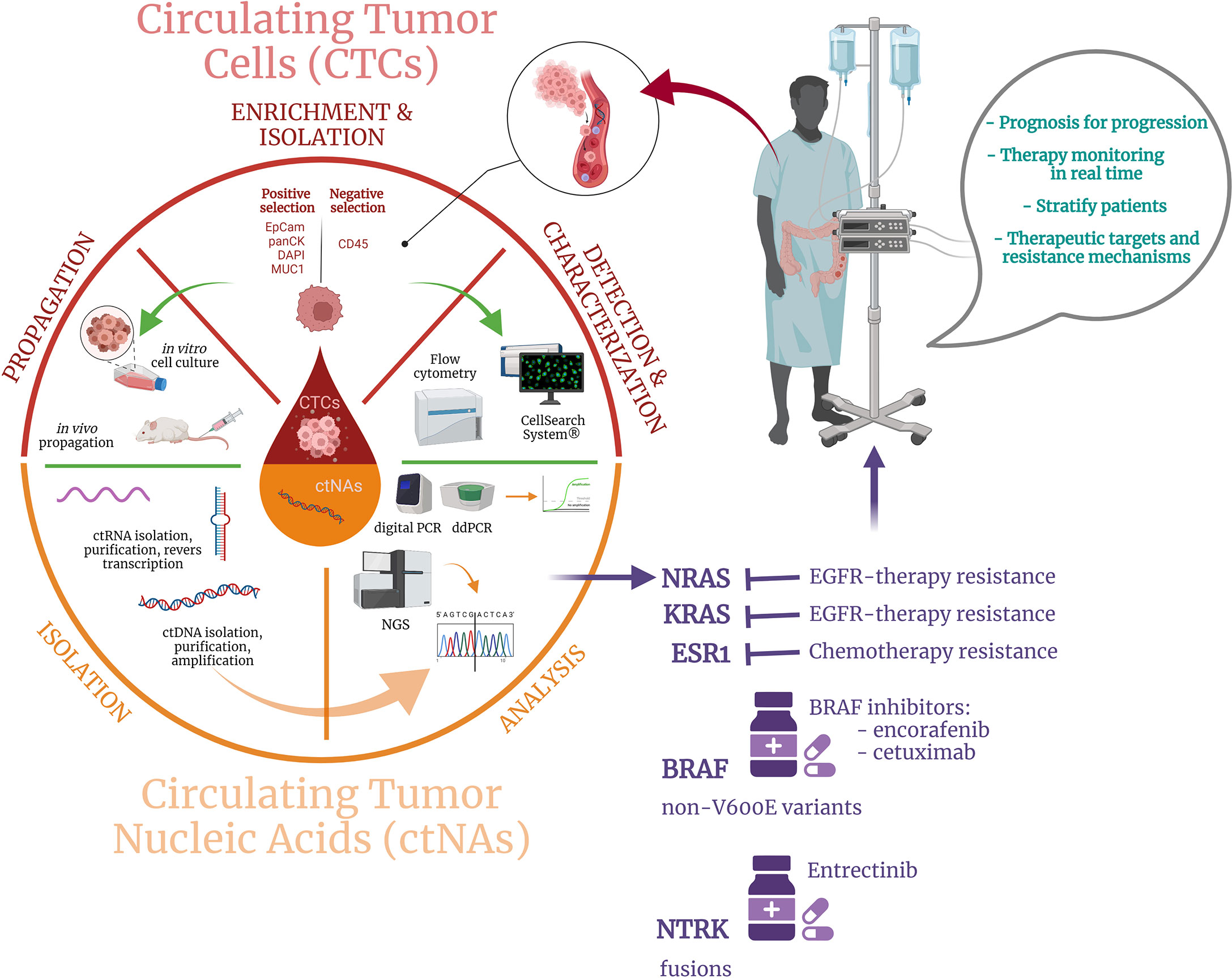
National Institutes of Health (NIH) funding plays a critical role in nurturing biomedical innovation in the U.S., despite present concerns over potential cuts to funding. Since its establishment, the NIH has been instrumental in providing grants and support that fuel groundbreaking research projects in various medical disciplines. This federal funding not only stimulates advancements in fundamental science but also catalyzes their translation into clinical applications, ensuring that discoveries benefit public health. The partnership between the NIH and academic institutions fosters a rich environment for experimentation and innovation, which has historically led to significant medical advancements, such as breakthroughs in cancer therapy and infectious disease management.
However, recent discussions around NIH funding cuts raise alarm among stakeholders, as reduced financial support could cripple the momentum of progress achieved over decades. The potential impact of these cuts could reverberate through the biomedical landscape, hindering the ability of researchers to explore innovative ideas and limiting the availability of resources for critical studies. The articulation of a sustainable funding model that protects and enhances NIH support is crucial to maintaining the vitality of the health innovation ecosystem and ensuring continued growth and success in biomedical research.
Lessons from World War II: Innovation in Warfare and Health
The experiences of World War II offer profound insights into the relationship between technological innovation in warfare and advancements in health. Historical analysis reveals that during the war, combatants faced not only the challenge of enemy forces but also the overwhelming threat of infectious diseases that ravaged troops. The creation of the OSRD was a direct response to this dual challenge, as it spurred innovation that ultimately led to life-saving medical breakthroughs such as the mass production of penicillin. This confluence of military demand and scientific endeavor underscored the necessity of a robust health innovation ecosystem capable of responding to urgent public health needs in the context of warfare.
These wartime innovations significantly reduced infection rates among soldiers, illustrating how crises can accelerate technological advancements. The historical precedent set during World War II demonstrates the effectiveness of mobilizing scientific resources in response to pressing health concerns, ultimately leading to the establishment of enduring structures for collaboration across sectors. Today, the same principles apply; recognizing the interconnectedness of warfare technology and health innovation can inform strategies to enhance current research initiatives and partnerships, benefiting both military personnel and civilian populations alike.
Technological Advancements from War to Wellness
Technological advancements born out of warfare have frequently been repurposed to enhance civilian health systems. The antibiotic revolution, which has its roots in World War II research, serves as a quintessential example. As scientists sought to confront the health crises presented by wartime injuries and infections, they developed innovative medical solutions that would prove invaluable long after the conflict ended. Penicillin’s transformation from a laboratory curiosity to a critical drug showcases how wartime urgency can precipitate significant strides in biomedical technology, highlighting the dynamic relationship between military needs and civilian healthcare advancements.
Moreover, technologies developed during wartime often yield unforeseen benefits for civilian domains. For instance, advancements in medical devices and diagnostic tools, spurred by military medical needs, have found applications in everyday healthcare settings. This dual-use technology principle emphasizes the ongoing role of defense-related research in fostering innovations that directly improve public health outcomes. Understanding and harnessing this relationship remains vital in navigating future challenges, ensuring that health innovation continues to thrive in both military and civilian sectors.
Balancing Indirect Costs in Research Funding
Indirect costs play a pivotal role in the sustainability of research funding, particularly within public-private partnerships in the biomedical sector. Understanding the historical context of indirect cost reimbursement under the OSRD illustrates the necessity to incentivize collaboration among private companies and academic institutions in military research. By covering these costs, the government enabled organizations to redirect their resources toward national health crises without bearing additional financial burdens, thereby fostering robust participation in research endeavors. This model has proven to be essential for expanding the frontiers of knowledge and advancing health innovation.
Today, as discussions regarding NIH funding cuts surface, the debate around indirect costs has resurfaced, highlighting the complex dynamics of resource allocation within health research. Balancing direct funding meant for specific projects with adequate support for overhead expenses is crucial to maintain a productive research environment. Establishing a system that ensures full and fair reimbursement for indirect costs can empower institutions to focus on scientific inquiries that yield transformative health outcomes, reinforcing the longstanding partnership between government funding and biomedical innovation.
The Future of the U.S. Health Innovation Ecosystem
Looking ahead, the sustainability of the U.S. health innovation ecosystem hinges on continued investment, collaboration, and adaptation to emerging challenges. As the landscape of healthcare evolves with technological advancements and shifting demographics, integrating diverse stakeholders—including academia, government, and industry—will be essential in addressing future health crises. Policymakers must prioritize robust funding mechanisms, creating an environment where innovative research can flourish, particularly in the face of concerns over budget constraints and diminishing NIH support.
Moreover, fostering a culture of collaboration amidst these sectors is vital for cultivating new ideas and translating research findings into practical applications. As we face global health challenges such as pandemics and antibiotic resistance, the lessons learned from historical partnerships must guide contemporary strategies. This proactive approach will not only preserve the U.S. position as a leader in health innovation but also ensure that the benefits of research translate into improved health outcomes for all.
Innovative Technologies for Future Healthcare Solutions
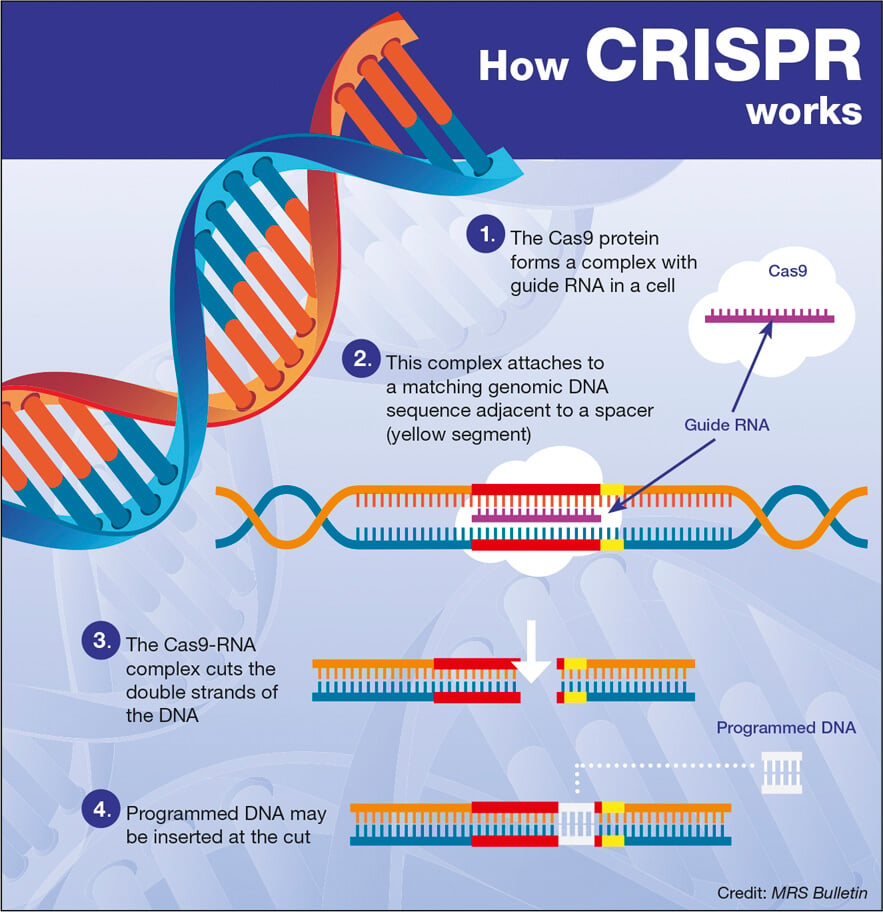
The intersection of technology and healthcare is rapidly evolving, with innovative solutions paving the way for a new era in health delivery. Emerging technologies such as artificial intelligence, telemedicine, and biotechnology are reshaping how clinicians diagnose and treat illnesses. The explosion of data analytics and machine learning offers unprecedented opportunities to personalize healthcare, improving patient outcomes through tailored treatment plans. These advancements have the potential to revolutionize traditional models of care, emphasizing preventative measures and patient engagement in health management.
As the U.S. health innovation ecosystem continues to embrace new technologies, key public-private research partnerships will be crucial in navigating these changes. Collaborations between academic institutions and tech companies can breed innovative approaches to old challenges, enhancing the efficiency and accessibility of healthcare services. As we look toward the future, leveraging advancements derived from a strong foundation of research and development will be instrumental in addressing persisting health disparities and ensuring that quality healthcare remains within reach for all.
Frequently Asked Questions
What role did public-private research partnerships play in the U.S. health innovation ecosystem?
Public-private research partnerships have been instrumental in shaping the U.S. health innovation ecosystem. Emerging during World War II, these collaborations enabled federal funding to boost academic research, resulting in significant advancements in biomedical innovation. This partnership model facilitated the rapid development of crucial medical technologies and therapies, laying the groundwork for today’s successful health innovation landscape.
How have NIH funding cuts impacted the U.S. health innovation ecosystem?
NIH funding cuts pose a significant threat to the U.S. health innovation ecosystem by potentially limiting financial resources for critical research projects. These cuts can disrupt public-private research partnerships that drive biomedical innovation, leading to fewer breakthroughs in medical technology and negatively impacting overall healthcare advancement.
What were the contributions of World War II medical advancements to the U.S. health innovation ecosystem?
World War II medical advancements were pivotal for the U.S. health innovation ecosystem, as they fostered a new approach to public-private research partnerships. The urgent need for effective medical solutions, such as the mass production of penicillin, highlighted the importance of collaboration between government, academia, and industry, setting the stage for continued innovation in medicine and public health.
In what ways has technology in warfare influenced the U.S. health innovation ecosystem?
Technology in warfare has significantly influenced the U.S. health innovation ecosystem by necessitating rapid medical advancements. The challenges faced during conflicts, particularly World War II, encouraged development in biomedical technologies and treatments, reinforcing the importance of collaborative public-private research efforts to address urgent healthcare needs.
Why is the U.S. health innovation ecosystem considered the envy of the world?
The U.S. health innovation ecosystem is regarded as the envy of the world due to its unique blend of strong public-private research partnerships, substantial NIH funding, and a rich history of biomedical innovation. These elements foster a robust infrastructure that consistently produces groundbreaking medical advancements, ensuring that the U.S. remains a leader in global health innovation.
| Key Points | |||||
|---|---|---|---|---|---|
| The U.S. health innovation ecosystem is a collaboration between the federal government, academia, and private industries that began during WWII. | Federal investments in research have historically supported medical advancements and technology. | The partnership emerged to address urgent wartime needs, leading to significant breakthroughs including the mass-production of penicillin. | The OSRD coordinated wartime research that has since shaped the landscape of biomedical innovation in the U.S. | The ongoing relationship between universities, the NIH, and the pharmaceutical industry is crucial for sustaining innovation. | Recent concerns over funding cuts to research could jeopardize this successful collaboration and its outcomes. |
| Research during WWII significantly reduced casualty rates from infectious diseases among soldiers. | The war prompted new policies for R&D, including federal funding for indirect costs, which remains important today. | The innovations fostered during WWII laid the groundwork for a thriving postwar biomedical field. | Future generations of scientists benefited from wartime research efforts, directly influencing the field of biomedicine. | Maintaining the current ecosystem is crucial for sustaining advancements that benefit both the U.S. and global health. |
Summary
The U.S. health innovation ecosystem is a dynamic and collaborative network that has evolved since World War II, fostering advancements in medicine and technology that serve as a model worldwide. The significant investment of federal funds into research has been a critical catalyst for breakthroughs in biomedical sciences. As we analyze the strengths and challenges of this ecosystem, it is crucial to recognize the importance of ongoing support for research and development, ensuring that the U.S. remains at the forefront of health innovation. The preservation and enhancement of this collaborative model will be vital for addressing contemporary health challenges and nurturing future discoveries.