Medical gaslighting is a burgeoning concern in today’s healthcare landscape, where patients often leave their doctor’s office feeling unheard or dismissed. This phenomenon occurs when symptoms are invalidated, potentially impacting the doctor-patient communication crucial for effective treatment and understanding. Particularly for individuals suffering from long COVID symptoms and other hard-to-diagnose conditions, the psychological impact of illness can be compounded by such invalidation. As healthcare burnout becomes increasingly prevalent among providers, the risk of miscommunication and emotional disconnect only escalates. Recognizing the significance of compassionate discourse in healthcare is essential to mitigate this troubling trend.
In recent discussions surrounding patient care and provider interactions, the concept often referred to as “medical invalidation” has gained traction, highlighting the challenges patients face when their experiences are dismissed. This issue, closely tied to doctor-patient communication, reflects a critical gap in understanding between individuals seeking help and physicians who may be overwhelmed by workload pressures. As healthcare systems grapple with burnout among medical professionals, it’s vital to explore how these dynamics contribute to the misunderstanding of conditions, especially in cases like long COVID. The emotional toll of not being believed can lead to significant psychological repercussions for patients, necessitating a shift towards more empathetic engagement in clinical settings. Addressing these forms of invalidation not only improves patient trust but also fosters a healthier environment for both patients and practitioners.
Understanding Medical Gaslighting in Healthcare
Medical gaslighting is a term that has gained significant traction in recent years, especially as patients face an increasing number of difficult-to-diagnose conditions. This phenomenon occurs when doctors dismiss or invalidate a patient’s symptoms, suggesting that they are either fabricated or exaggerated. The psychological impact of such experiences can be profound, leading to a breakdown of trust between patient and provider. Patients with long COVID symptoms or irritable bowel syndrome often feel marginalized and misunderstood, which can exacerbate their condition. The recognition of medical gaslighting is essential for improving doctor-patient communication, as it highlights the need for empathetic and attentive care.
While the discussion around medical gaslighting often emphasizes the negative experiences of patients, it is crucial to understand the pressures faced by healthcare providers that might contribute to these invalidations. Factors such as high caseloads and the burden of documentation can limit a doctor’s ability to engage fully with their patients. When physicians are pressed for time, their focus may shift from truly listening to patients towards simply providing rushed responses. This dynamic can lead to misunderstandings and, ultimately, the feeling of being gaslighted on the part of the patient. Therefore, creating an environment where providers feel less pressure to perform can significantly improve the accuracy of diagnoses and the quality of interactions.
The Role of Healthcare Burnout and Its Impact on Patient Care
Healthcare burnout is a significant issue that not only affects the well-being of healthcare providers but also has far-reaching consequences for patient care. With over half of practicing physicians experiencing burnout, the quality of doctor-patient communication can deteriorate. Burnout leads to emotional exhaustion and can cause healthcare professionals to become disengaged during patient interactions. When doctors are overwhelmed, they may inadvertently communicate ineffectively or dismissively, making patients feel invalidated or unheard. Addressing burnout through organizational changes and support systems is crucial to restoring compassion and empathy in healthcare settings.
Moreover, understanding the factors contributing to burnout, such as administrative burdens and ever-increasing patient demands, is essential for developing lasting solutions. Healthcare organizations need to prioritize the mental health of their staff as passionately as they do for their patients. By implementing systems that reduce the workload and improve work-life balance for healthcare professionals, we create a more sustainable healthcare environment. This not only enhances the well-being of the providers but also leads to improved patient outcomes, as more engaged and fulfilled doctors are better positioned to recognize and validate the concerns of their patients.
Addressing Medical Invalidation to Improve Patient Experiences
Medical invalidation, as distinguished from gaslighting, refers to the phenomenon where a healthcare provider fails to acknowledge a patient’s symptoms or experiences, often resulting in feelings of frustration and alienation among patients. This is particularly evident in cases where patients suffer from complex or largely misunderstood conditions, such as chronic fatigue syndrome or fibromyalgia. By labeling these experiences as medical invalidation rather than gaslighting, healthcare professionals can more accurately address the root of the problem without assuming harmful intent. This reframing fosters a better understanding of the emotional toll on patients and encourages more empathetic responses from providers.
Creating awareness around medical invalidation can lead to significant improvements in patient outcomes. By training healthcare providers to recognize how their attitudes and communication styles influence patient experiences, we can mitigate the negative effects of invalidation. This education should include active listening techniques, empathy training, and strategies for acknowledging patients’ lived experiences, particularly in vague or challenging medical presentations. By prioritizing this aspect of care, healthcare providers can foster a more supportive environment that empowers patients to voice their concerns without fear of dismissal.
Building Trust through Empathetic Doctor-Patient Communication
One of the cornerstones of effective healthcare is trust, which is built through empathetic doctor-patient communication. When patients feel heard and understood, they are more likely to engage in open dialogue and adhere to treatment plans. Empathy allows healthcare professionals to connect with their patients on a personal level, bridging gaps created by the complexities of medical conditions and the pressures of the healthcare system. By validating patients’ experiences and feelings, doctors can promote a more cooperative and supportive relationship that enhances healing.
To cultivate an atmosphere of trust, providers should focus on active listening and personalized care strategies. This includes making an effort to pause during consultations, allowing patients space to explain their symptoms without interruption. Additionally, doctors can employ open-ended questions that encourage patients to express their concerns openly. Such techniques work to dismantle barriers that might lead to feelings of invalidation and help ensure that patients feel valued. Ultimately, this improved communication can foster better health outcomes and patient satisfaction.
The Psychological Impact of Illness on Patients
Being diagnosed with a chronic illness can have a significant psychological impact on patients, often leading to feelings of anxiety, depression, and helplessness. This emotional burden can be compounded when patients experience invalidation from their doctors. The perception that their symptoms are not taken seriously or are deemed psychological can exacerbate feelings of isolation. Understanding the psychological impact of illness is key for healthcare providers, as it highlights the importance of addressing not just the physical symptoms but also the emotional and psychological well-being of patients.
To mitigate these effects, healthcare professionals must adopt a holistic approach to patient care that encompasses both physical and mental health. This can mean integrating mental health support within primary care settings to ensure patients receive comprehensive care. Encouraging self-advocacy among patients can also empower them, reducing feelings of helplessness and promoting a sense of agency in managing their condition. By recognizing the multidimensional impact of illness, healthcare providers can foster a more supportive environment that matches the needs of their patients.
Exploring Long COVID Symptoms and Patient Experiences
Long COVID is a complex and evolving condition characterized by a range of symptoms that persist long after the initial infection. Patients suffering from long COVID often report a variety of troubling symptoms—ranging from fatigue and cognitive difficulties to respiratory issues—that can drastically affect their quality of life. As healthcare providers struggle to fully understand and diagnose these symptoms, patients may find themselves facing medical invalidation, where their lived experiences are not acknowledged or taken seriously. This situation underscores the critical need for open lines of communication and a more concerted effort to validate patient experiences.
The exploration of long COVID symptoms should be met with a compassionate approach from healthcare providers who should encourage open dialogue and acknowledge the myriad of experiences that patients are undergoing. Understanding that each patient may have unique symptomatology requires a shift towards individual-centered considerations in healthcare. By employing empathetic practices and focused attention on the patient’s narrative, providers can engage in a more constructive discussion about symptoms, treatment options, and management strategies. Ultimately, a commitment to validating and understanding long COVID experiences can lead to improved patient satisfaction and health outcomes.
Enhancing Doctor-Patient Relationships Through Better Communication Strategies
Doctor-patient relationships thrive when communication is prioritized. Effective communication strategies can transform the healthcare experience for both patients and providers. Techniques such as reflective listening and validating expressions of concern can significantly enhance interpersonal dynamics. When healthcare professionals actively engage with their patients and acknowledge the emotional weight of their symptoms, they foster an atmosphere of trust and collaboration. The result is a partnership where patients feel safe to share their concerns, which is essential for accurate diagnosis and treatment.
Incorporating regular feedback mechanisms into consultations can further enhance communication. Encouraging patients to share their feelings about the consultation process can provide invaluable insights for healthcare providers. This bidirectional communication is vital in addressing any feelings of doubt or invalidation, ensuring both parties are heard. Furthermore, investing in communication training for healthcare teams can cultivate a culture of empathy, slowly shifting organizational practices towards a more patient-centered approach that honors both the emotional and physical aspects of health.
Advocating for System-Level Changes to Reduce Pressures on Healthcare Providers
The structural challenges within healthcare systems can significantly affect provider performance and, consequently, patient care. Organizations need to advocate for system-level changes that prioritize a healthier work environment for physicians and healthcare staff. Streamlining administrative processes and reducing unnecessary paperwork can alleviate some of the burdens contributing to healthcare burnout. When providers are supported in their roles, they are better equipped to offer genuine attention and care during patient interactions, thus reducing instances of medical invalidation.
Moreover, fostering a supportive culture within healthcare organizations can empower providers to speak openly about their struggles, creating a feedback loop that encourages continuous improvement. Initiatives that focus on mental health, resilience training, and team-building activities can foster solidarity among healthcare workers, making them feel valued and supported. Ultimately, by implementing these supportive structures, healthcare systems can improve the overall experience for both providers and patients alike, firmly establishing a culture of compassion and quality care.
The Future of Patient-Centric Care in Medicine
The evolving landscape of healthcare is increasingly recognizing the importance of patient-centric care. As the focus shifts toward treating patients as partners in their health journeys, it is vital for providers to harness new communication strategies and empathetic practices. Technology can play a significant role here, with telehealth solutions and digital platforms facilitating access to care while allowing for more personal interactions. By integrating these tools effectively, healthcare providers can enhance patient engagement, leading to improved health outcomes and patient satisfaction.
Moreover, patient-centric care emphasizes the importance of understanding the patient’s perspective and incorporating their feedback into the treatment process. This paradigm shift not only validates patient experiences but empowers individuals, allowing them to take an active role in managing their health. As healthcare continues to evolve, there is a promising outlook for the integration of practices that nourish the mind and body, yielding greater resilience against challenges like medical invalidation and healthcare burnout.
Frequently Asked Questions
What is medical gaslighting and how does it relate to patient experiences in healthcare?
Medical gaslighting refers to situations where patients feel dismissed or invalidated by healthcare providers regarding their symptoms or conditions. It often manifests when doctors cannot find a concrete cause for a patient’s illness, leading to suggestions that symptoms may be psychological. This form of medical invalidation can significantly affect patient outcomes, especially in cases like long COVID symptoms, where patients feel their experiences are not taken seriously.
How does healthcare burnout contribute to medical gaslighting?
Healthcare burnout among providers can lead to medical gaslighting. When physicians face overwhelming caseloads and time pressures, they may struggle to engage empathetically with patients. This can result in quick dismissals of valid concerns, leaving patients feeling unheard and invalidated. Thus, addressing healthcare burnout is essential to improving doctor-patient communication and reducing instances of medical gaslighting.
What are the psychological impacts of medical gaslighting on patients?
Patients experiencing medical gaslighting often suffer from psychological impacts, including anxiety, depression, and a diminished sense of self-worth. The feeling of being invalidated can lead to distrust in medical professionals, exacerbating their health issues. By understanding the nuances of doctor-patient communication, we can better support those affected by this harmful practice.
How can patients advocate against medical gaslighting during their doctor visits?
To combat medical gaslighting, patients should prepare for doctor visits by documenting their symptoms clearly and expressing their concerns assertively. Asking clarifying questions, seeking second opinions, and bringing a trusted friend or family member to appointments can help ensure their experiences are validated and taken seriously.
What alternatives to the term ‘medical gaslighting’ are preferred by healthcare professionals?
Many healthcare professionals prefer the term ‘medical invalidation’ over ‘medical gaslighting’ because it emphasizes the lack of intent behind dismissive behaviors. This perspective encourages compassion for providers who are often overwhelmed rather than labeling these interactions as malicious, thus fostering a more constructive dialogue regarding patient care.
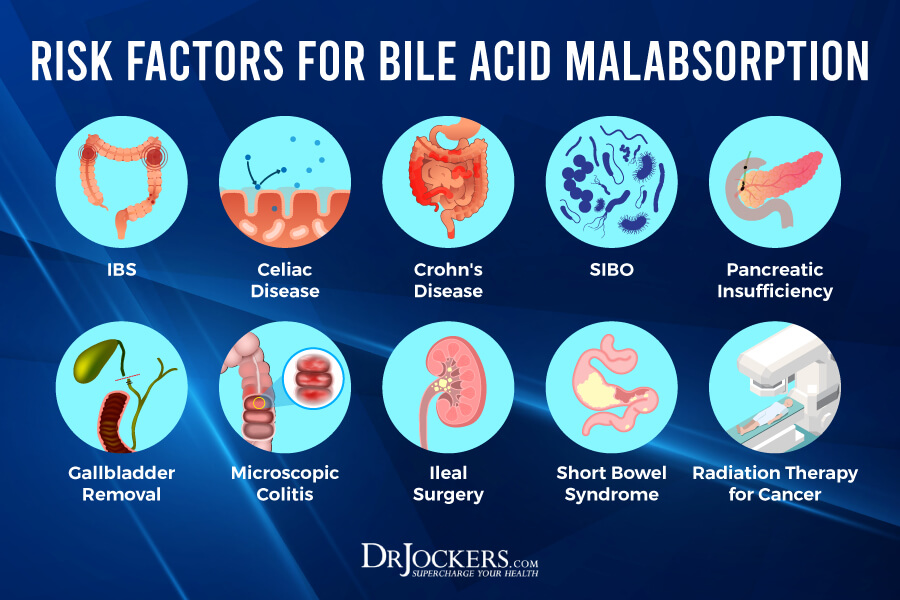
Are there specific conditions that are often associated with medical gaslighting?
Yes, conditions such as long COVID, irritable bowel syndrome, and chronic pain disorders are frequently associated with medical gaslighting. Patients with these hard-to-detect ailments may feel invalidated when their symptoms are not corroborated by standard medical tests, highlighting the importance of empathetic doctor-patient communication.
How can improvements in doctor-patient communication reduce instances of medical gaslighting?
Enhancing doctor-patient communication can significantly reduce medical gaslighting. Creating an open dialogue where patients feel safe to express their symptoms, combined with providers taking the time to listen and validate their experiences, fosters trust and supports better health outcomes. Implementing training programs that focus on empathy and communication skills in medical education can be beneficial.
What role does social media play in highlighting issues of medical gaslighting?
Social media has amplified discussions surrounding medical gaslighting, providing a platform for patients to share their experiences and connect with others facing similar challenges. This visibility can raise awareness among healthcare providers about the impact of medical invalidation and encourage systemic changes to improve patient care.
What systemic changes can be made to address medical gaslighting in healthcare?
To combat medical gaslighting, systemic changes such as reducing provider workloads, increasing time allotted for patient visits, and fostering a culture of empathy in healthcare settings are necessary. By easing the pressures that lead to burnout, healthcare organizations can support providers in delivering more attentive and affirming patient care.
How can recognizing the signs of medical invalidation benefit patients’ health outcomes?
Recognizing signs of medical invalidation empowers patients to seek clarification and assert their needs effectively. By understanding that their feelings are valid and seeking supportive care, patients can advocate for themselves better, leading to improved health outcomes and strengthened relationships with their healthcare providers.
| Key Points | Details |
|---|---|
| Definition of Medical Gaslighting | Medical gaslighting refers to the phenomenon where patients feel dismissed or invalidated by healthcare providers regarding their symptoms, particularly when conditions are hard to diagnose. |
| Pressures on Providers | Healthcare professionals face heavy caseloads and documentation pressures, which can limit their ability to fully engage with and validate patients’ experiences. |
| Intent vs. Invalidation | Psychologist Alexandra Fuss suggests that much of what is termed medical gaslighting may not be intentional, and may be better described as ‘medical invalidation’. |
| Role of Social Media | The concept of medical gaslighting has gained visibility on social media, leading to increased awareness and discussion on invalidating patient experiences. |
| Impact of Time Constraints | Time limitations during patient visits can hinder the ability of doctors to ask empathetic questions, potentially leaving patients feeling ignored. |
Summary
Medical gaslighting is a significant concern in healthcare today, as patients often leave medical appointments feeling dismissed or invalidated regarding their symptoms. This phenomenon arises from various pressures within the healthcare system, including high caseloads, extensive documentation requirements, and a lack of time for meaningful patient interactions. While the term ‘gaslighting’ implies a malicious intent, many instances of medical gaslighting may actually stem from systemic issues rather than deliberate actions by medical providers. Understanding and addressing this problem, especially through compassion and support for both patients and healthcare professionals, is crucial in fostering better health outcomes.