The safety of patients in medical research is paramount, as their well-being is intrinsically linked to the integrity of the entire research process. Institutional Review Boards (IRBs) play a critical role in ensuring patient safety in studies by meticulously reviewing and overseeing research protocols, safeguarding against ethical breaches. With federal research funding increasingly susceptible to cuts and freezes, like the recent $2 billion halt at Harvard, there is growing concern about how these disruptions could compromise medical research oversight. When funding is threatened, the resources and infrastructure necessary for effective IRB protocols may falter, ultimately putting participants at risk. In an era of heightened clinical research ethics, prioritizing patient safety remains essential for fostering public trust and advancing scientific discovery.
Ensuring the welfare of participants in scientific trials is a cornerstone of ethical medical research. This responsibility falls significantly on the governance provided by review boards, which assess research projects to mitigate risks and ensure compliance with ethical standards. As funding for research initiatives faces cuts, the consequences ripple through the system, affecting the mechanisms designed to protect those who volunteer for clinical trials. The implications reach far beyond immediate oversight, touching on broader themes of trust in the research community and the future of healthcare innovation. In light of these developments, it is crucial to maintain a focus on the protection and rights of individuals involved in medical studies.
Understanding the Critical Role of IRB Protocols in Patient Safety
Institutional Review Boards (IRBs) play an indispensable role in ensuring patient safety in medical research by meticulously reviewing all research proposals and procedures. These boards ensure compliance with ethical guidelines and legal regulations, thereby protecting the rights and welfare of participants involved in clinical trials. Each proposed study undergoes rigorous scrutiny, where factors such as the clarity of the research question, the adequacy of informed consent procedures, and the assessment of potential risks and benefits are comprehensively evaluated. The IRB’s authority ensures that no study can proceed without first addressing these essential issues, ultimately safeguarding participants from potential harm.
Moreover, IRBs are responsible for ongoing oversight throughout the various stages of a research study. This includes monitoring adverse events, participant recruitment strategies, and ensuring that informed consent is properly maintained. By providing a structured review process, IRBs help to establish public trust in medical research, which is crucial for the ongoing support and participation of individuals in these studies. Their ability to uphold ethical standards not only protects current participants but also sets a precedent that reinforces the integrity of human subjects research moving forward.
The Impact of Funding Cuts on Clinical Research Ethics
Recent federal funding cuts have far-reaching implications for clinical research ethics, particularly in the context of patient safety. The halt of funding prevents IRBs and research institutions from conducting comprehensive reviews and oversight necessary for the protection of study participants. Resources that traditionally support ethical oversight and staff training are now in jeopardy, which can lead to inadequate reviews and potential oversights in patient safety protocols. This disrupts the fundamental ethical framework established to protect human subjects in medical studies, raising concerns about the integrity of ongoing and upcoming research.
Furthermore, the cessation of grants hampers institutions’ ability to maintain the essential infrastructures that promote ethical research practices, including training programs for researchers and staff. These programs are vital for preparing professionals to navigate the complex ethical considerations inherent in clinical research. Without adequate funding, the risk of compromising patient safety increases, potentially leading to adverse outcomes that could have been avoided with proper oversight and resources.
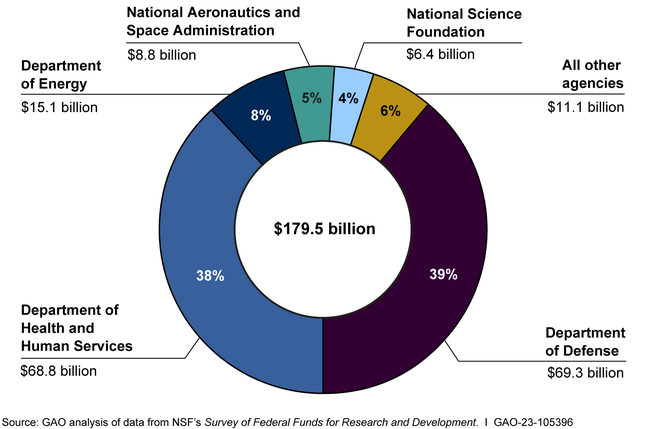
Federal Research Funding: A Lifeline for Patient Protection
Federal research funding serves as a critical lifeline for projects aimed at maintaining patient safety in medical research. Grants from organizations like the National Institutes of Health (NIH) not only support the research itself but also provide the financial backing necessary for maintaining robust oversight mechanisms through IRBs. This funding facilitates the development and implementation of rigorous protocols that ensure the safety and welfare of participants in clinical trials, enabling researchers to adhere to high ethical standards.
When funding is disrupted, the entire framework that upholds patient protection can be precariously affected. From hiring trained staff to conducting important safety monitoring, each aspect of research ethics relies on this financial support. Reduction in available funds can lead to diminished capacity for compliance with established protocols, increasing the risk of errors and ethical oversights that compromise participant safety. Thus, maintaining and securing adequate funding is crucial for the continuity of ethical practices in medical research.
The Consequences of Research Disruptions on Patient Trust
Disruptions in medical research funding can significantly erode public trust in the research community, especially concerning patient safety in studies. When ongoing research is halted or delayed, potential participants may become skeptical about the commitment of researchers to uphold safety protocols. Historical cases of research misconduct have created a legacy of mistrust that can resurface whenever ethical oversight is believed to be compromised.
As trust wavers, patients may be less willing to participate in clinical trials, leading to fewer opportunities for advancing medical knowledge and treatments. This reluctance can exacerbate health disparities as marginalized communities become increasingly wary of research practices that have historically overlooked their rights and welfare. To counteract this potential fallout, it is essential for research institutions to recommit to transparency and ethics, reinforcing the importance of safeguarding patient safety even amidst funding uncertainties.
Ethics Training and Its Importance in Clinical Research
Ethics training is crucial in equipping researchers and IRB members with the knowledge and skills necessary to prioritize patient safety in medical research. This training emphasizes the need to understand the ethical implications of research proposals, including the importance of informed consent, risk assessment, and participant welfare. Providing researchers with a strong ethical foundation is essential for ensuring that studies are designed and implemented with consideration for the rights of participants.
Furthermore, ongoing training ensures that research professionals are aware of new regulations and ethical guidelines that continue to evolve. As research methodologies and technologies advance, so too must the ethical frameworks that govern research practices. By investing in substantial ethics training, research institutions reaffirm their commitment to protecting human subjects, thereby ensuring a culture of safety and trust within the research community.
The Role of Community Engagement in Research Ethics
Community engagement plays a pivotal role in reinforcing the ethics of medical research and enhancing patient safety. Actively involving community members in the research process—whether through advisory boards or public consultations—ensures that the interests and concerns of potential participants are front and center. This connection fosters mutual trust, promoting transparency in how research aims to benefit the community while adequately protecting its members.
Additionally, involving the community can help researchers identify unique cultural and social factors that may influence participants’ perceptions of safety and risk in clinical trials. By taking these factors into account, research design can be adjusted to better meet the needs of the population served. Engaging with communities not only strengthens ethical oversight but also contributes to more effective and relevant research outcomes.
Historical Context of Patient Safety in Clinical Trials
Understanding the historical context of patient safety in clinical trials is fundamental for appreciating the development of current ethical practices in medical research. Past injustices, such as the Tuskegee Syphilis Study and the Willowbrook hepatitis studies, highlight the necessity for robust ethical oversight in research involving human subjects. These events led to the establishment of rigorous IRB protocols and regulations designed to prevent similar ethical breaches in the future.
Today, the legacy of these historical events continues to inform contemporary research practices and illuminate the critical importance of protecting patient safety. The establishment of laws and ethical standards has fostered an environment in which the rights and well-being of research participants are paramount, fundamentally enhancing the integrity of clinical trials. Acknowledging these lessons from the past is essential in guiding the ethical direction of future research efforts.
Innovations in Clinical Trials Promoting Patient Safety
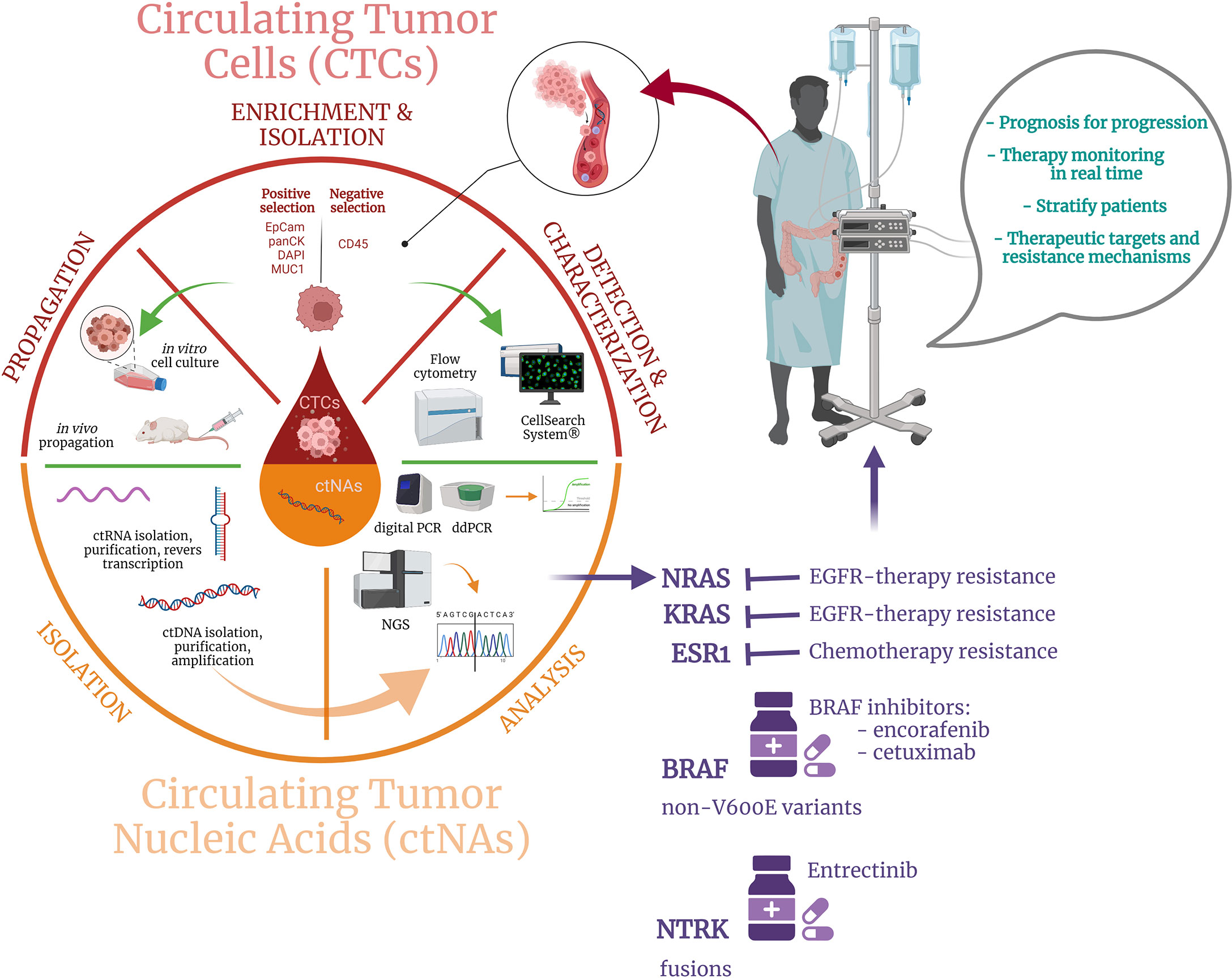
Innovative approaches in clinical trials are constantly evolving, presenting new ways to enhance patient safety in medical research. For instance, the use of technology, such as remote monitoring systems, has transformed how data is collected and analyzed, allowing for real-time tracking of participants’ health and safety. Such advancements make it easier for IRBs to ensure that studies comply with safety protocols while also addressing potential risks more proactively.
Moreover, innovations in patient-engagement strategies—such as using digital platforms to facilitate informed consent and communicate trial updates—foster transparency and support participant autonomy. These developments empower participants by enhancing their understanding of processes, allowing for better-informed choices regarding their involvement. Ultimately, integrating innovative practices not only augments the ethical considerations in clinical research but also prioritizes the safety of all individuals participating in studies.
Future Directions in Patient Safety and Ethical Research Oversight
Moving forward, the landscape of patient safety in medical research will increasingly rely on adaptive models of ethical oversight that respond to evolving societal expectations and technological advancements. As patient engagement becomes more integral to research design, IRBs will need to adapt their protocols to encompass diverse voices and perspectives, ensuring that patient safety remains the focal point of clinical trials.
Additionally, surge in digital health technologies and telemedicine research paradigms can potentially streamline ethical reviews and enhance patient protection mechanisms. However, such advancements must be approached with caution, as the need for rigorous ethical scrutiny continues to grow with the complexity of modern research. Continuous learning and adaptation within the context of research ethics will be imperative in safeguarding participant welfare while advancing medical knowledge.
Frequently Asked Questions
What are the key mechanisms that ensure the safety of patients in medical research?
The safety of patients in medical research is primarily ensured through Institutional Review Boards (IRBs), which review, approve, and monitor research studies involving human participants. They evaluate the research design, informed consent processes, risk assessments, and the overall ethical framework to minimize potential harm to patients.
How do IRB protocols contribute to the safety of patients in medical studies?
IRB protocols play a crucial role in safeguarding patients by establishing comprehensive guidelines for ethical research practices. They assess the proposed studies for potential risks, ensure informed consent is obtained, and monitor ongoing research to protect the rights and welfare of participants throughout the study period.
In what ways does federal research funding support patient safety in clinical trials?
Federal research funding supports patient safety in clinical trials by providing the necessary resources for rigorous oversight and compliance with ethical standards. Funding initiatives often require adherence to IRB review processes, thereby enhancing the protection and rights of research participants across multiple sites.
What impact do funding cuts have on the oversight of patient safety in medical research?
Funding cuts can severely hinder the oversight of patient safety in medical research by disrupting IRB operations and limiting resources available for monitoring studies. This can lead to delays in patient recruitment, increased risks during studies, and reduced public trust in the research community.
How does medical research oversight improve patient safety in studies?
Medical research oversight improves patient safety by enforcing ethical standards through IRB reviews, monitoring adverse events, and ensuring that researchers fulfill their obligations to protect participants. This oversight also fosters transparency, accountability, and public trust in the research process.
What are the ethical considerations for ensuring patient safety in medical research?
Ethical considerations for ensuring patient safety in medical research include obtaining informed consent, conducting thorough risk-benefit analyses, providing transparency about research processes, and fostering an environment of respect and care for all participants involved in the studies.
How do collaboration and oversight mechanisms enhance patient safety in clinical research?
Collaboration among research institutions, supported by effective oversight mechanisms like SMART IRB, enhances patient safety by streamlining ethical reviews across multiple sites, reducing redundant processes, and facilitating faster responses to emerging risks, thus maintaining a high standard of care for participants.
Why is it essential to uphold strong safety measures for patients participating in medical research?
Upholding strong safety measures for patients in medical research is essential to prevent potential harms, foster public trust, and ensure ethical standards are met. The history of medical research highlights the importance of safeguarding participant rights and well-being to maintain the integrity and credibility of clinical studies.
| Key Points | Details |
|---|---|
| Impact of Funding Freeze | Over $2 billion in federal research grants to Harvard halted, disrupting safety and rights of patients in studies. |
| Role of SMART IRB | Facilitates oversight of multi-site medical research to protect patients’ rights and welfare. |
| Importance of IRBs | Review proposals, assess risks, and ensure informed consent to protect patient safety in research. |
| Historical Context | Past medical abuses led to the establishment of IRBs to uphold ethical research conduct. |
| Consequences of Cuts | Cuts to funding risk the safety of research participants and damage public trust in medical research. |
Summary
The safety of patients in medical research is paramount to uphold ethical standards and public trust. Recent funding cuts have severely impacted oversight systems like SMART IRB, jeopardizing the protection of patient rights in multi-site studies. This disruption not only halts essential research but also reinforces skepticism about clinical trials, potentially deterring future participation. To safeguard the welfare of patients, it is crucial to maintain robust funding and support for research oversight mechanisms that ensure ethical practices in all medical investigations.