Pediatric cancer recurrence remains a significant concern for families navigating the challenging landscape of childhood oncology. In a groundbreaking study, researchers have developed an artificial intelligence (AI) tool that outperforms traditional methods in predicting the risk of relapse in young patients, particularly those with gliomas. This advancement in cancer imaging technology utilizes temporal learning to analyze longitudinal brain scans, providing vital insights into the likelihood of recurrence. By improving our understanding of relapse patterns, we aim to enhance care strategies in pediatric oncology, ultimately aiming to reduce the emotional and physical burden on children and their families. With these innovative approaches, including AI in medicine, we are one step closer to transforming pediatric cancer management and outcomes.
When discussing the challenges associated with the return of childhood cancers, it is important to consider factors such as relapse in young patients and the complexities of managing their treatment journeys. Advanced predictive models now use AI advancements to better assess the potential for glioma recurrence, a type of brain tumor commonly seen in pediatric cases. By leveraging cancer imaging technology and methods like temporal learning, researchers are exploring novel ways to provide earlier warnings about the possibility of relapse. Such solutions are pivotal for pediatric oncology, allowing healthcare professionals to tailor interventions based on individual risk factors. Overall, the integration of AI into medical strategies paves the way towards more effective management of pediatric cancer and its aftermath.
Advancements in Pediatric Oncology Through AI
Artificial Intelligence (AI) is transforming the landscape of pediatric oncology, particularly in how we predict cancer outcomes. With traditional methods often falling short, the integration of AI in medicine is proving revolutionary. AI tools, such as those developed at Mass General Brigham, harness vast amounts of data, enabling them to analyze multiple brain scans over time. This innovative approach stands in stark contrast to conventional techniques, which typically rely on single imaging results. By employing advanced algorithms, these tools can deliver more accurate predictions concerning the relapse risks associated with pediatric cancers.
Moreover, the application of AI in predicting disease trajectories represents a pivotal shift in patient management strategies. As noted in recent studies, including those focusing on glioma prediction, AI can facilitate earlier interventions and personalized treatment plans. The capability to forecast potential recurrences empowers healthcare providers to make informed decisions, thereby enhancing the quality of care for young patients. With ongoing research and clinical trials, the future of pediatric oncology looks promising as AI continues to break new ground in treatment and monitoring strategies.
Understanding Pediatric Cancer Recurrence Risks
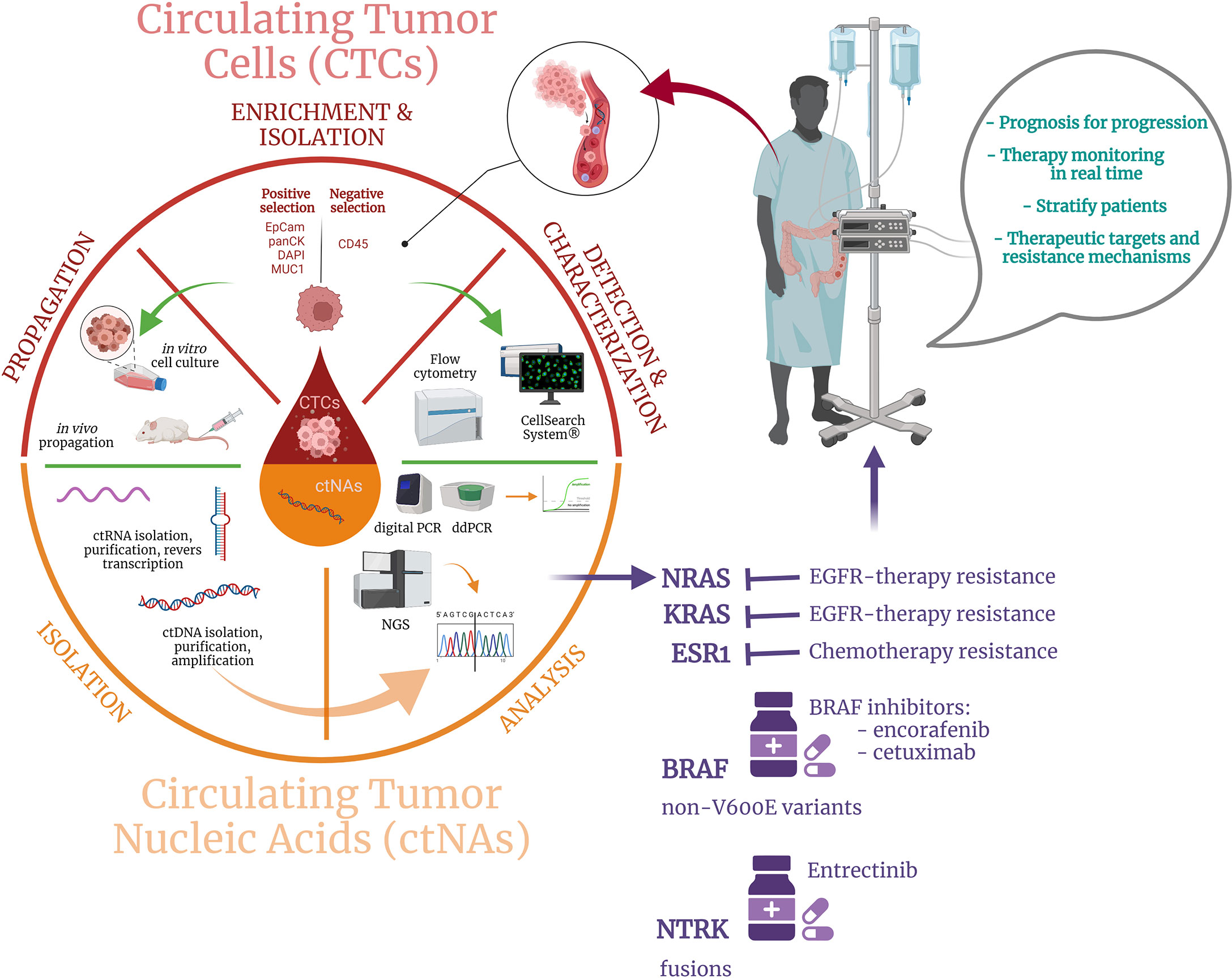
Pediatric cancer recurrence poses a significant challenge in the realm of child health and oncology. Notably, gliomas, a type of brain tumor prevalent among children, have varying degrees of risk associated with their recurrence. Understanding these risks is crucial for medical professionals and families navigating the complexities of treatment. Recent advancements, particularly those utilizing cancer imaging technology, have shed light on predictive markers that can signal potential relapses. This understanding is vital, as the psychological and physical toll on young patients and their families can be profound in the event of recurrence.
Researchers are increasingly turning to tools like temporal learning in AI to refine the accuracy of these predictions. By examining multiple MRI scans over time, healthcare providers can identify subtle changes that may indicate heightened risks of recurrence. This innovative approach not only improves the prediction accuracy but can also inform treatment decisions. If pediatric cancer recurrence risks can be assessed more accurately, clinicians may be able to tailor follow-up care more effectively, ensuring that patients receive the appropriate level of monitoring without unnecessary stress.
The Role of Temporal Learning in Cancer Imaging
Temporal learning represents a groundbreaking technique in cancer imaging, especially as it pertains to pediatric oncology. Traditionally, AI models analyzed images as static snapshots, which limited their effectiveness in recognizing evolving tumor characteristics. However, temporal learning changes the game by incorporating a sequence of images acquired over time. This methodology allows AI to comprehend progressive changes in a patient’s brain scans, which are crucial for predicting pediatric cancer recurrence. By applying a temporal lens, researchers can train models that not only detect immediate signs of recurrence but also forecast future risks based on historical data.
The application of temporal learning thus enhances the predictive power of AI-driven models. For instance, in clinical trials conducted at Mass General Brigham, using multiple scans significantly improved the accuracy of glioma risk predictions to between 75-89%. This advancement is critical, as it supports clinicians in making proactive decisions about patient care. As AI continues to evolve and integrate with established cancer imaging technology, the hope is that these models can lead to timely interventions, guiding the course of treatment to mitigate the chances of relapse rather than merely responding to existing tumors.
The Importance of MRI in Predicting Cancer Outcomes
Magnetic Resonance Imaging (MRI) is pivotal in managing pediatric cancers, particularly when monitoring for recurrence. As children often require prolonged follow-ups to assess their recovery from tumors like gliomas, MRI serves as a non-invasive tool for capturing relevant data. However, the stress associated with frequent imaging can weigh heavily on young patients and their families. By leveraging advancements in AI and imaging technology, researchers aim to make these procedures more informative and less daunting.
Incorporating AI into the MRI analysis process can streamline patient follow-up protocols and enhance the understanding of what the imaging reveals about potential cancer recurrence. With improved algorithms analyzing multiple scans, healthcare providers can discern patterns that may have previously gone unnoticed. Thus, MRI becomes not just a tool for observation, but an integral part of a precision medicine approach that tailors follow-up care based on the most accurate risk assessments available.
Future Directions in Pediatric Cancer Management
The future of pediatric cancer management looks promising, thanks to the rapid developments in AI technology and its application in oncology. As researchers continue to refine tools for predicting cancer outcomes, the emphasis on personalized treatment strategies grows stronger. By integrating AI’s capabilities with established healthcare frameworks, clinicians can offer streamlined care tailored to individual patient needs, ultimately improving outcomes for children with cancers like gliomas.
Moreover, ongoing studies aim to validate AI’s predictive accuracy across diverse settings, thereby laying the groundwork for broader clinical applications. As tools evolve, the goal remains to reduce healthcare burdens on families while enhancing the quality of care. Future trials may focus on the practical implementation of AI-informed predictions in clinical routines, potentially transforming current practices in pediatric oncology and offering new hope for managing pediatric cancer recurrence.
Enhancing Care through AI-Driven Insights
AI-driven insights are transforming the landscape of pediatric oncology, providing tools that can significantly enhance care practices. By analyzing historical data from thousands of MRI scans, researchers can identify patterns that inform decision-making processes about treatment and monitoring protocols. This leap in capability allows clinicians to classify patients based on recurrence risk more accurately, tailoring interventions that align with an individual child’s specific needs.
The implications of this transformation extend beyond mere accuracy; they encompass improving the overall patient experience. Reducing the frequency of imaging for lower-risk patients can alleviate stress for children and their families, addressing an often-overlooked aspect of cancer treatment. The effort to implement these AI-driven strategies represents a commitment to not only advancing technological capabilities but also to enhancing the holistic approach to pediatric cancer care.
Key Takeaways on AI and Pediatric Cancer
From the integration of AI in medical imaging to advancements in predictive modeling, the implications for pediatric cancer care are profound. One key takeaway is that predictive tools developed with advanced technology offer a means to enhance the accuracy of identifying risks associated with pediatric cancer recurrence, especially in conditions like gliomas. The potential for these tools to reshape clinical pathways could lead to more effective management strategies and improved outcomes for young patients.
Another essential consideration is the ethical and practical implications of implementing AI in clinical settings. As we navigate these new technologies, it is crucial to maintain a patient-centered focus, ensuring that advancements in predictive capabilities are aligned with compassionate care for affected families. Continued research and validation will be essential in transitioning these AI tools from experimental to routine clinical use, thereby maximizing their benefits to pediatric oncology.
The Challenges Ahead in AI Implementation
While the advances in AI for predicting pediatric cancer outcomes show great promise, several challenges need to be addressed. One significant hurdle is the need for robust datasets that encompass diverse demographics and clinical scenarios to ensure AI models are not only accurate but also equitable. Collaborations across institutions can help in pooling data, but keeping patient privacy and ethical considerations at the forefront is crucial to successful implementation.
Additionally, there is the challenge of integrating AI tools into existing healthcare systems. Clinicians will need training and support to effectively utilize these advanced models, ensuring they can interpret AI outputs meaningfully in the context of individual patient care. Bridging the gap between technology and practical application will require ongoing dialogue between AI researchers and clinical practitioners to develop user-friendly interfaces and workflows that enhance rather than complicate patient management.
The Future of Pediatric Oncology Research
The future of pediatric oncology research is bright, particularly with the integration of innovative technologies like AI. By advancing how researchers understand and predict cancer behavior, studies not only pave the way for improved patient outcomes but also inspire new directions for therapeutics. The synergy between clinical findings and machine learning could unlock new insights into tumor biology, opening avenues for targeted therapies that mitigate severe risks like recurrence.
As ongoing research builds on the findings from institutions like Mass General Brigham, the collaborative approach can lead to comprehensive models that encompass not only imaging but also genetic and biomolecular data. This multifaceted perspective will be instrumental in designing precision medicine that addresses the unique challenges presented by pediatric cancers. Future research will undoubtedly continue to focus on refining AI applications, ultimately contributing to happier and healthier outcomes for children facing cancer.
Frequently Asked Questions
What is pediatric cancer recurrence and how does it relate to gliomas?
Pediatric cancer recurrence refers to the return of cancer in children after treatment. In the context of gliomas, which are common brain tumors in children, recurrence can be particularly challenging. Many pediatric gliomas can be effectively treated with surgery; however, understanding and predicting the risk of recurrence is essential for managing patient care.
How does AI improve predictions of pediatric cancer recurrence?
AI improves predictions of pediatric cancer recurrence by analyzing multiple brain scans over time rather than relying solely on single images. This approach allows for a more nuanced understanding of changes in the brain, enabling better predictions about the likelihood of relapse in pediatric cancer patients, particularly those with gliomas.
What is temporal learning and how does it contribute to predicting pediatric cancer recurrence?
Temporal learning is a technique used in AI that synthesizes information from consecutive imaging studies over a period. By analyzing MRI scans taken at different times, the AI can identify subtle changes that may indicate a higher risk of pediatric cancer recurrence, thereby improving prediction accuracy for conditions like gliomas.
Why is predicting pediatric cancer recurrence so challenging?
Predicting pediatric cancer recurrence is challenging due to the variability in individual cases and the complex nature of cancers like gliomas. Traditional methods often rely on single imaging scans for decisions, which can lead to inaccuracies. The need for more reliable assessment tools is critical for improving patient outcomes.
What are the implications of using advanced imaging technology in pediatric oncology?
Advanced imaging technology, particularly when enhanced by AI, has significant implications in pediatric oncology. It can lead to earlier detection of potential recurrences in cancers like gliomas, which may result in timely interventions and improved treatment plans tailored to each patient, thereby optimizing overall care.
How does the study on AI predict pediatric cancer recurrence affect treatment protocols?
The findings from the study highlight the potential for AI tools to refine treatment protocols in pediatric oncology by identifying patients who are at high risk for recurrence. This could allow clinicians to customize surveillance strategies, possibly reducing the frequency of imaging for lower-risk patients while enabling proactive measures for those at a higher risk.
What role does imaging technology play in managing the risk of pediatric cancer recurrence?
Imaging technology is critical in managing the risk of pediatric cancer recurrence as it provides essential data to monitor changes in tumors post-treatment. Enhanced imaging, especially through AI analytics, can improve the accuracy of these assessments, leading to better informed decisions regarding follow-up care in pediatric patients.
What are the future prospects for AI in predicting pediatric cancer recurrence?
The future of AI in predicting pediatric cancer recurrence is promising, particularly with ongoing research and validation of models like those using temporal learning. As these technologies are further developed, they could transform how pediatric oncologists assess risks and tailor therapies, ultimately improving outcomes for children battling cancers like gliomas.
| Key Point | Details |
|---|---|
| AI Tool Effectiveness | A novel AI tool surpasses traditional methods in predicting relapse risk in pediatric glioma patients. |
| Study Background | Conducted by researchers at Mass General Brigham, Boston Children’s Hospital, and Dana-Farber, leveraging 4,000 MRI scans from 715 patients. |
| Temporal Learning Technique | The AI uses temporal learning, analyzing multiple scans over time to improve accuracy. |
| Prediction Accuracy | The model predicts cancer recurrence with 75-89% accuracy, significantly better than the 50% accuracy of single-image analyses. |
| Clinical Applications | Further validation is required, with hopes to implement AI-driven predictions in clinical trials to enhance patient care. |
Summary
Pediatric cancer recurrence is a significant concern for families dealing with childhood gliomas, but advances in AI technology are changing the landscape of risk prediction. A new study reveals that an AI tool can predict recurrence risks in pediatric patients with a much higher accuracy than traditional methods. This innovative approach not only promises to enhance the care provided to affected children but also aims to alleviate the stress of frequent imaging follow-ups, by providing a clearer understanding of patient risks. As research progresses, there’s hope that these developments will lead to improved treatment pathways for pediatric cancer patients facing the threat of recurrence.